Assessment and Investigations:
Management
Assessment and Investigations
Management
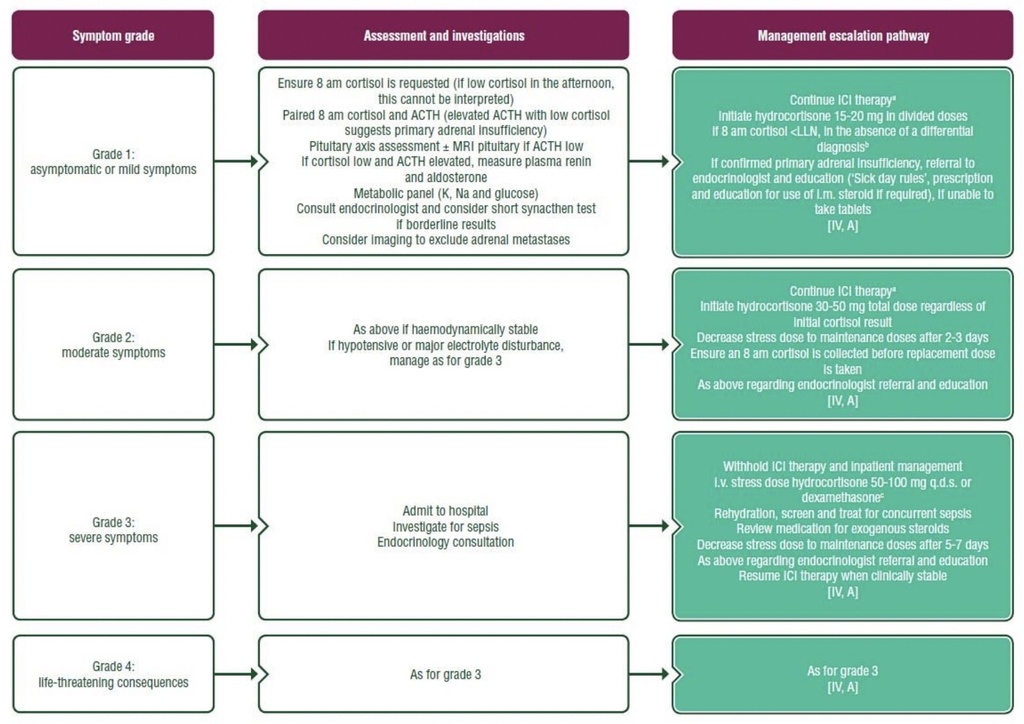
Purple: general categories or stratification; turquoise: combination of treatments or other systemic treatments; white: other aspectsof management. ACTH, adrenocorticotrophic hormone; HRT, hormone replacement therapy; ICI, immune checkpoint inhibitor; i.v. intravenous; K,potassium; LLN, lower limit of normal; MRI, magnetic resonance imaging; Na, sodium; q.d.s., four times a day.
a Maintenance HRT in divided doses: 15-20 mg hydrocortisone; if intercurrent illness, higher doses will be required; if symptomatic,initiation at double the standard dose may be required, with a plan to wean down over 7 days, if a patient is not able to adhere to a short-acting steroid regimen. Hydrocortisone 20 mg is equivalent to prednisone 5 mg. Diagnostic measures should never delay the initiation of steroid replacement therapy in suspected adrenal insufficiency. In primary adrenal insufficiency, mineralocorticoid replacement is also indicated (0.1 mg per day of fludrocortisone) — seek endocrinologist advice.
b Differential diagnoses of low cortisol, i.e. with high ACTH: adrenalitis; with low ACTH: hypophysitis, pituitary tumour or exogenousadrenal suppression, e.g. from concurrent steroid use (e.g. dexamethasone >0.75 mg, prednisolone >3 mg; also consider steroidinhalers).
c Dexamethasone emergency replacement may be useful in cases where the diagnosis of primary adrenal insufficiency issuspected as it will interfere less with assessment of an ACTH stimulation test.