Clinical presentation
Recommendations:
Early flexible rectosigmoidoscopy or ileocolonoscopy with biopsies in patients with suspected IRenterocolitis of grade >1 is strongly recommended.
Endoscopie findings:
Endoscopic features include erythema, erosion, ulceration and luminal bleeding, although normal colon mucosa can be present in 40% of patients despite grade 2 symptoms of colitis.
Deep ulcerations and extensive inflammation above the left colon are predictive of CS-refractory disease and requirement for immunosuppressant treatment.
IR-microscopic colitis is a separate entity. It causes chronic watery diarrhoea in patients treated with anti-PD-1 or anti-
CTLA-4 therapy. The endoscopic appearance of IRmicroscopic colitis is either normal or shows mild erythema or oedema. There are two main forms: lymphocytic colitis (intraepithelial lymphocytosis and infiltration of the lamina propria) and the less common collagenous colitis(thickening of the collagen subepithelial layer).
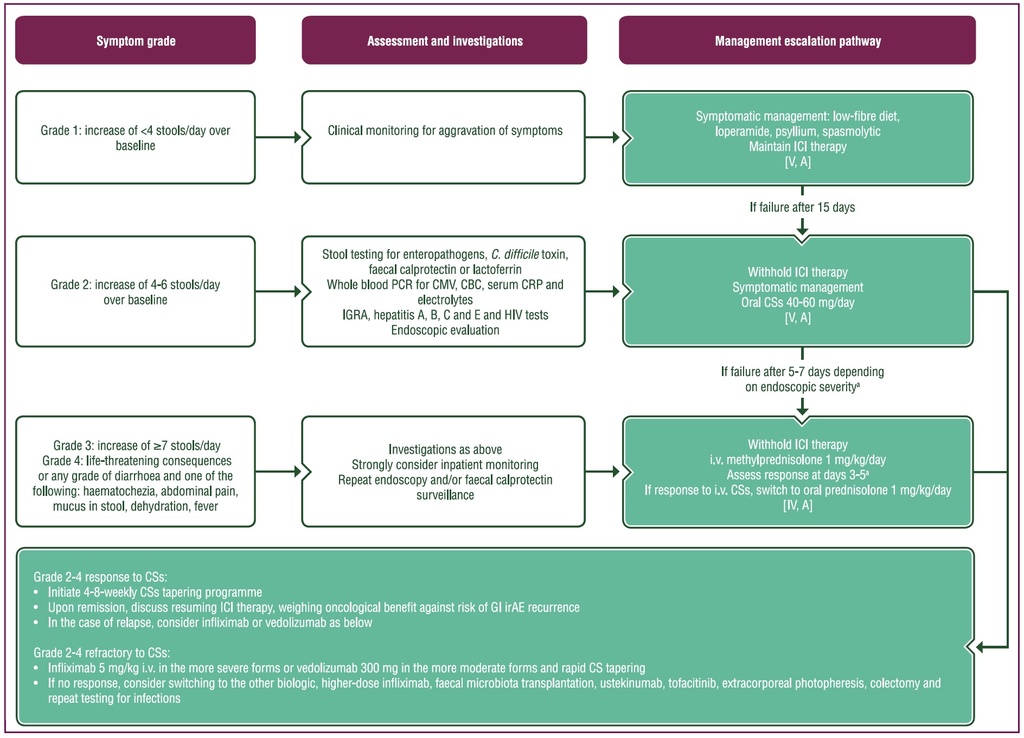
Purple: general categories or stratification; turquoise: combination of treatments or other systemic treatments; white: other aspects of management.
C. difficile, Clostridioides difficile; CBC, complete blood count; CMV, cytomegalovirus; CRP, C-reactive protein; CS, corticosteroid; GI, gastrointestinal; HIV, human immunodeficiency
virus; ICI, immune checkpoint inhibitor; IGRA, interferon-gamma release assay; IR, immune-related; irAE, immune-related adverse event; i.v., intravenous.
aIn cases of extensive colitis and ulcerations or high levels of faecal calprotectin (>400 mg/mg), if colonoscopy is not available.
IR-upper GI tract injury is not as common as IR-enterocolitis and may involve the oral cavity (stomatitis), oesophagus, stomach and duodenum. The predominant upper GI symptoms are nausea, vomiting, dysphagia, odynophagia, haematemesis and abdominal pain. Upper GI inflammation can be isolated or associated with enterocolitis.
Endoscopic findings:
Endoscopic findings include erythema, erosions and ulcerations.
Histology:
Histological inflammation of the stomach and the duodenum, with or without clinical symptoms, has been reported in 50%-75% of patients with GI irAEs. Gastric biopsies show intraepithelial lymphocytosis and inflammatory infiltrate with neutrophils. Duodenal biopsies show partial (rarely total) villous blunting, crypt distortion, intraepithelial lymphocytosis and eosinophilic, lymphocytic and plasma-cell infiltration of the lamina propria.
Management:
Upper GI inflammation is often patchy and mild; in most cases, it can be managed effectively with proton-pump inhibitors (PPIs).
Severe forms with deep gastric ulcerations, however, may require CSs or biologics
Source:
Management of toxicities from immunotherapy: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up
Published online: 18 October 2022
J. Haanen, M. Obeid, L. Spain et al, on behalf of the ESMO Guidelines Committee