IR-pulmonary toxicities are a group of heterogeneous diseases including different clinical entities such as the frequent IR-interstitial lung disease (IR-ILD) or IRpneumonitis and other rare entities such as IRbronchiolitis or IR-lung sarcoidosis.
In general, symptoms include dyspnoea, cough, chest pain, fever and hypoxia.
Radiological patterns of IR-ILD have been classified into five possible subtypes: cryptogenic organising pneumonia-like, groundglass opacities, interstitial, hypersensitivity and pneumonitis not otherwise specified.
Several histopathological findings have been reported for IRILD, including cellular interstitial pneumonitis, organising pneumonia and diffuse alveolar damage, while sometimes only minimal abnormalities can be identified. Nevertheless, it is important that any pathognomonic radiological or pathological features are clearly identified.
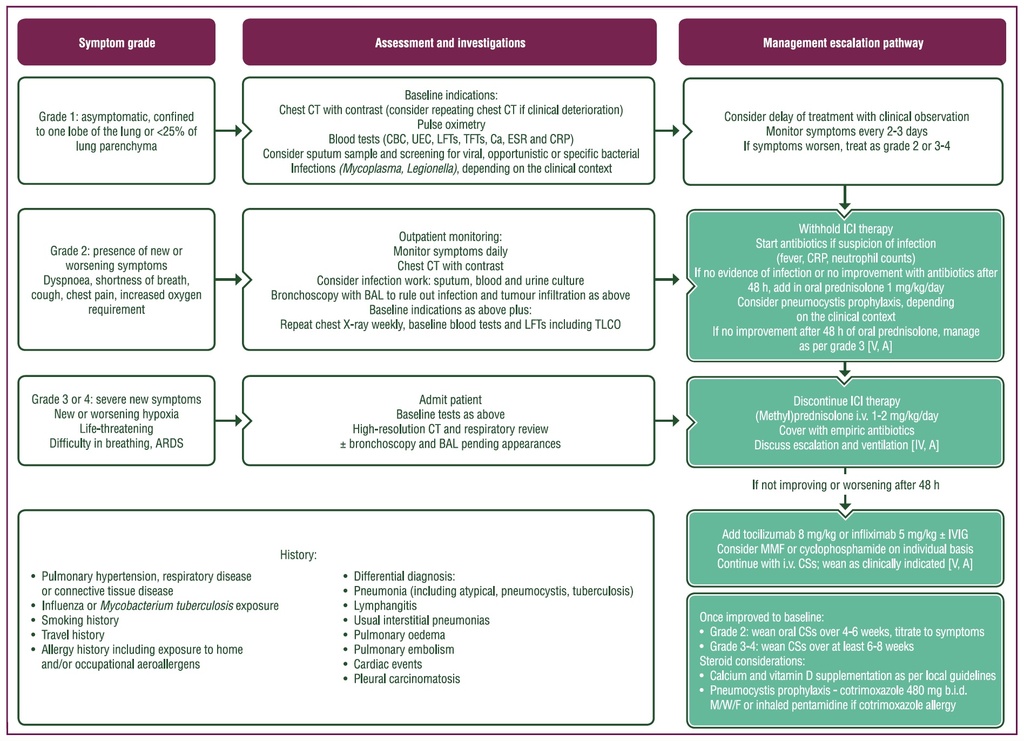
Purple: general categories or stratification; turquoise: combination of treatments or other systemic treatments; white: other aspects of management.
ARDS, acute respiratory distress syndrome; BAL, bronchoalveolar lavage; b.i.d., twice daily; Ca, calcium; CBC, complete blood count; CRP, C-reactive protein; CS,
corticosteroid; CT, computed tomography; ESR, erythrocyte sedimentation rate; ICI, immune checkpoint inhibitor; ILD, interstitial lung disease; IR, immune-related; i.v.,
intravenous; IVIG, intravenous immunoglobulin; LFT, liver function test; MMF, mycophenolate mofetil; M/W/F, Monday,Wednesday and Friday; TLCO, transfer capacity
of the lung for carbon monoxide; TFT, thyroid function test; UEC, urea and electrolytes.
Source:
Management of toxicities from immunotherapy: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up
Published online: 18 October 2022
J. Haanen, M. Obeid, L. Spain et al, on behalf of the ESMO Guidelines Committee