The diagnosis of ircAEs is usually based on clinical evaluation when a simple, non-complicated rash is observed; this can be facilitated by skin biopsy and more specific tests, depending on the clinical presentation. Pathological examination of maculopapular rashes shows lymphocytic CD4þ infiltrates with eosinophils and papillary oedema. Lichenoid reactions are associated with a characteristic band of dense dermal lymphocytic infiltrate with degeneration and vacuolisation of the basal membrane.
In BP, direct immunofluorescence shows C3 and immunoglobulin (Ig) G deposits on the basal membrane, and serological testing for anti-basal membrane antibodies may show autoantibodies. Biopsies from vitiligo-like eruptions have shown CD4þ and CD8þ lymphocytes in close vicinity to apoptotic melanocytes. Psoriatic lesions present characteristic signs of a thickened and parakeratotic stratum corneum, elongated rete ridges and perivascular lymphocytic infiltration.
Although the vast majority of ircAEs are of mild or moderate severity, early (and repeated, if needed) evaluation of the disease severity should be carried out to eliminate rare severe irAEs such as StevenseJohnson syndrome, toxic epidermal necrolysis, bullous lesions and DRESS syndrome that necessitate immediate interruption of ICI therapy, specialist treatment and monitoring.
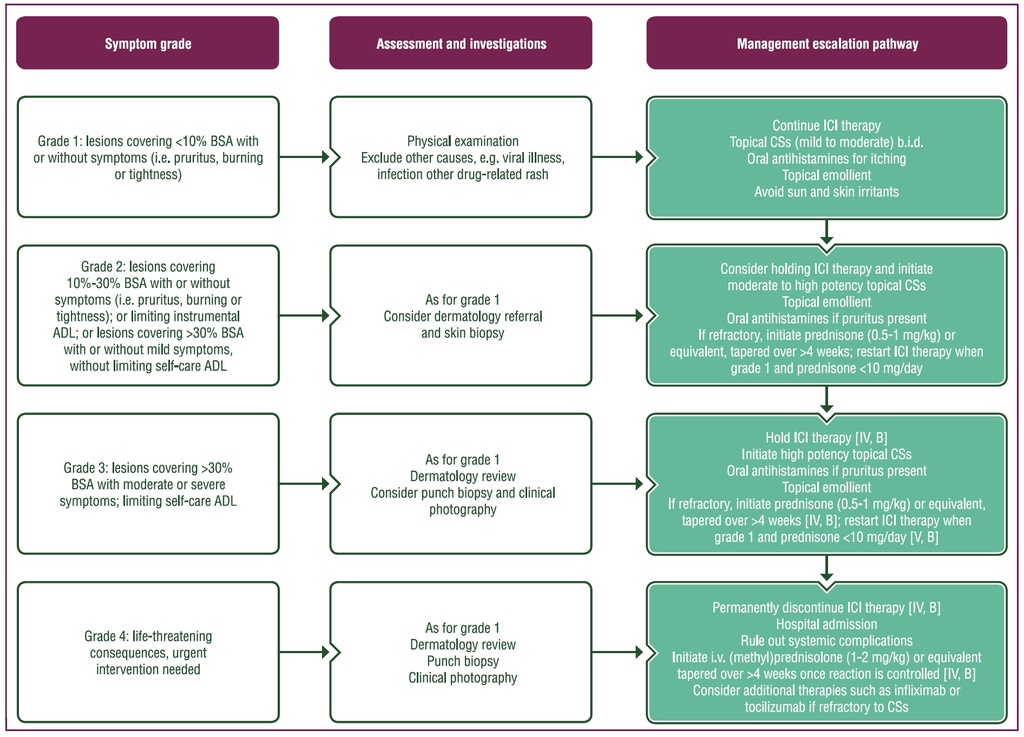
Purple: general categories or stratification; turquoise: combination of treatments or other systemic treatments; white: other aspects of management.
ADL, activities of daily living; b.i.d., twice daily; BSA, body surface area; CS, corticosteroid; ICI, immune checkpoint inhibitor; IR, immune-related; i.v., intravenous.
Source:
Management of toxicities from immunotherapy: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up
Published online: 18 October 2022
J. Haanen, M. Obeid, L. Spain et al, on behalf of the ESMO Guidelines Committee